Search
Guideline 6 – Compressions
Next review July 2024
Summary

Who does this guideline apply to?
This guideline applies to all persons who are unresponsive and not breathing normally.
Who is the audience for this guideline?
This guideline is for use by bystanders, first aiders or first aid providers, first responders and health professionals.
Recommendations
The Australian and New Zealand Committee on Resuscitation (ANZCOR) makes the following recommendations:
- All rescuers should perform chest compressions for all persons who are unresponsive and not breathing normally.
- Interruptions to chest compressions should be minimised.
- Those who are trained and willing to give rescue breaths do so for all persons who are unresponsive and not breathing normally.
Guideline

All rescuers should perform chest compressions for all persons who are unresponsive and not breathing normally.1,2 [Strong recommendation, moderate certainty of evidence] ANZCOR suggests that those who are trained and willing to give rescue breaths do so for all who are in cardiac arrest.1,2 [Weak recommendation, very-low-certainty evidence]
Recognition of the need for Chest Compressions

All rescuers, including health care professionals, should use unresponsiveness and absence of normal breathing to identify the need for resuscitation.1-4 [Good practice statement] Palpation of a pulse is unreliable and should not be performed to confirm the need for resuscitation.5-8 [Good practice statement]
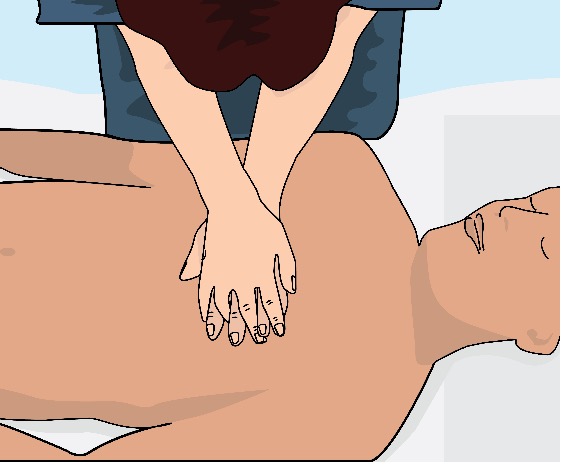
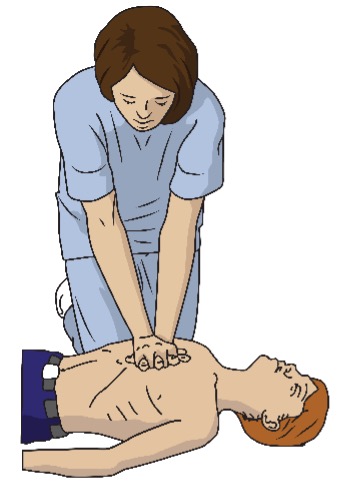
Locating the site for Chest Compressions

ANZCOR suggests performing chest compressions on the lower half of the sternum.1,2,4,9 [CoSTR 2015/2020, weak recommendation, very-low-certainty evidence] In making this recommendation, we place a high value on consistency with current treatment recommendations in the absence of compelling data suggesting the need to change the recommended approach.1,2,4,9 Place the heel of their hand in the centre of the chest with the other hand on top (Figure 1). [Good practice statement]
Avoid compression beyond the lower limit of the sternum. Compression applied too high is ineffective and if applied too low may cause regurgitation and/or damage to internal organs. [Good practice statement]
Figure 1: Location of chest compressions
Infants

In infants, ANZCOR suggests the two finger technique should be used by lay rescuers in order to minimise transfer time from compression to ventilation. Having obtained the compression point the rescuer places two fingers on this point and compresses the chest (Figure 2). [Good practice statement]
Figure 2: Method of compression for infants
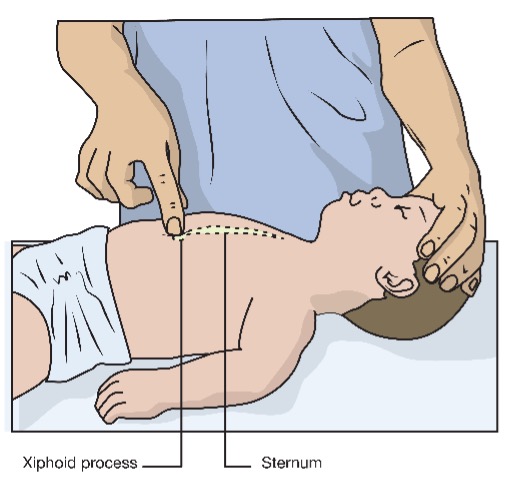
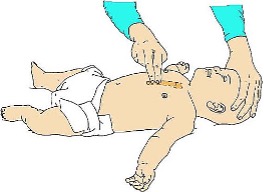
(adapted courtesy of European Resuscitation Council)
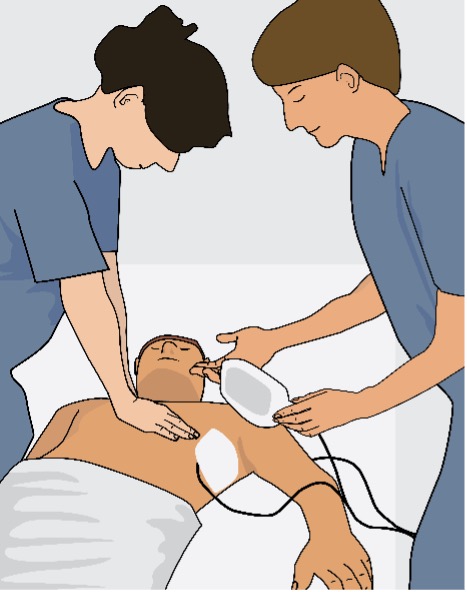
Children and Adults

Either a one or two hand technique can be used for performing chest compressions in children.5-8 (Figure 3) [Good practice statement]
Figure 3: Administering compressions using one- and two-handed techniques

(adapted courtesy of European Resuscitation Council)
Interruptions to chest compressions must be minimized.3,4 [2015 CoSTR, weak recommendation, low-quality evidence] A person requiring chest compressions should be placed on their back on a firm surface before commencing chest compressions to optimise the effectiveness of compressions.1,2,10 [2020 CoSTR, weak recommendation, very-low-certainty evidence] Compressions should be rhythmic with equal time for compression and relaxation. The rescuer must avoid either rocking backwards and forwards, or using thumps or quick jabs. Rescuers should allow complete recoil of the chest after each compression.1,2,11 [2020 CoSTR, weak recommendation, very-low-certainty evidence]
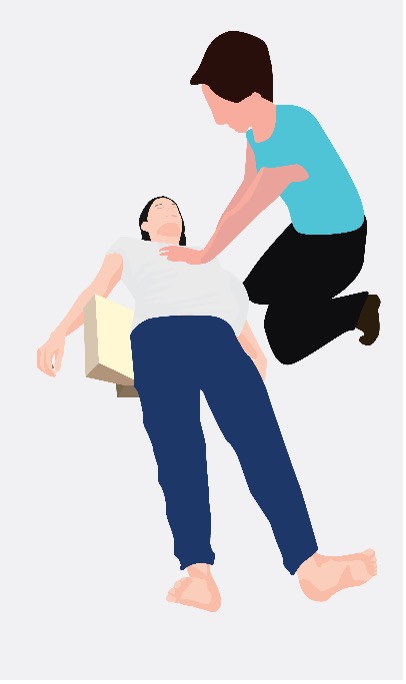
Pregnant women

There are no published studies of optimum positioning in pregnant women undergoing cardiopulmonary resuscitation (CPR) so recommendations to date are extrapolated from manikin studies or studies of pregnant women who are not in cardiac arrest. Good quality, uninterrupted chest compressions as described above should be the immediate priority in all pregnant women who are unresponsive and not breathing normally.1,2,4,9 [Good practice statement]
In noticeably pregnant women, standard CPR should be commenced immediately. Once CPR is in progress, if there are sufficient resources available, rescuers should place padding such as a towel, cushion or similar object under the right hip to tilt the woman’s hips (approximately 15-30 degrees) to the left but leave her shoulders flat to enable good quality chest compressions. The reason for this position in pregnant women is to move the weight of the pregnant uterus off of her major blood vessels in the abdomen. If a tilted position is not possible or tilting the hips compromises the quality of chest compressions, then chest compressions should be performed as described as above with the woman on her back.
Figure 4: Padding the noticeably pregnant woman
Depth of Compressions

The lower half of the sternum should be depressed approximately one third of the depth of the chest with each compression. This equates to more than 5cm in adults,1,2,4,9,11 approximately 5cm in children5,6,12,13 and 4 cm in infants.5,6,12,13 [2015/2020 CoSTR, weak recommendation, very-low-certainty evidence] ANZCOR places greater importance on adequate compression depth. Although there is some evidence suggesting detriment with compression depths greater than 6cm, the clinical reality of being able to tell the difference between 5 or 6 cm and adjust compressions accordingly is questionable. Inadequate compression depth is definitely associated with poor outcomes. ANZCOR has elected not to put an upper limit on compression depth as the risk of too shallow compressions outweighs the risk of compressions that are too deep.3,4 [Good practice statement]
Rate of Compressions

Rescuers should perform chest compressions for all ages at a rate of 100 to 120 compressions per minute (almost 2 compressions/second).1,2,4,9,11 [CoSTR 2015/2020, strong recommendation, very-low-certainty evidence] This does not imply that 100-120 compressions will be delivered each minute since the number will be reduced by interruptions for breaths given by rescue breathing. ANZCOR acknowledges that compression rates will vary between and within providers and survival rates are optimised at compressions rates of 100-120 compressions per minute. There is some evidence that compressions rates less than 100 or greater than 140 compressions per minute are associated with lower rates of survival.1,2,4,9,11
CPR Quality

The compression rate and depth is variable among rescuers and compressions may be worse in the first 5 minutes of the arrest.14 One manikin study of rescuer CPR showed that compressions became shallow within one minute, but providers became aware of fatigue only after 5 min.7 When performing compressions, if feasible, change rescuers at least every two minutes to prevent rescuer fatigue and deterioration in chest compression quality, particularly depth.1,2,15-17 [Good practice statement] Changing rescuers performing chest compressions should be done with a minimum of interruptions to compressions.14,17
Feedback

There is no high level evidence that the use of CPR feedback devices during real time CPR improves survival or return of spontaneous circulation.1-4 CPR prompt / feedback devices may be considered for clinical use to provide data as part of an overall strategy to improve quality of CPR at a systems level.1-4 [CoSTR 2015/2020, weak recommendation, very-low-certainty evidence]. ANZCOR places a higher value on resource allocation and cost effectiveness than widespread implementation of a technology with uncertain effectiveness during real time CPR. We acknowledge that data provided by CPR feedback devices may benefit other victims as part of a broader quality improvement system.1-4
Risks

Rib fractures and other injuries are common but acceptable consequences of CPR given the alternative of death.15 [Good practice statement] CPR should be initiated for presumed cardiac arrest without concerns of harm to patients not in cardiac arrest.3,4 [CoSTR 2015, strong recommendation, very-low-certainty evidence] In making this recommendation, ANZCOR places a higher value on the survival benefit of CPR initiated by laypersons for patients in cardiac arrest against the low risk of injury in patients not in cardiac arrest.3,4
References

- Olasveengen TM, Mancini ME, Perkins GD, et al. Adult Basic Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2020; 142(16_suppl_1): S41-S91.
- Olasveengen TM, Mancini ME, Perkins GD, et al. Adult Basic Life Support: International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2020; 156: A35-A79.
- Perkins GD, Travers AH, Berg RA, et al. Part 3: Adult basic life support and automated external defibrillation. 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2015; 95: e43-e69.
- Travers AH, Perkins GD, Berg RA, et al. Part 3: Adult Basic Life Support and Automated External Defibrillation 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2015; 132(16 suppl 1): S51-S83.
- Maconochie IK, Aickin R, Hazinski MF, et al. Pediatric Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2020; 142(16_suppl_1): S140-S84.
- Maconochie IK, Aickin R, Hazinski MF, et al. Pediatric Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2020; 156: A120-A55.
- de Caen AR, Kleinman ME, Chameides L, et al. Part 10: Paediatric basic and advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2010; 81(1): e213-e59.
- Kleinman ME, De Caen AR, Chameides L, et al. Part 10: Pediatric Basic and Advanced Life Support 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2010; 122(16 suppl 2): S466-S515.
- Perkins GD, Handley AJ, Koster RW, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. Resuscitation 2015; 95: 81-99.
- Holt J, Ward A, Mohamed T-Y, et al. The optimal surface for delivery of CPR: A systematic review and meta-analysis. Resuscitation 2020; 155: 159-64.
- Considine J, Gazmuri RJ, Perkins GD, et al. Chest compression components (rate, depth, chest wall recoil and leaning): A scoping review. Resuscitation 2020; 146(Jan): 188-202.
- Maconochie IK, de Caen AR, Aickin R, et al. Part 6: Pediatric basic life support and pediatric advanced life support 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2015; 95: e147-e68.
- De Caen AR, Maconochie IK, Aickin R, et al. Part 6: Pediatric Basic Life Support and Pediatric Advanced Life Support. Circulation 2015; 132(16 suppl 1): S177-S203.
- Wik L, Kramer-Johansen J, Myklebust H, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. Jama 2005; 293(3): 299-304.
- Koster RW, Sayre MR, Botha M, et al. Part 5: Adult basic life support: 2010 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 2010; 81(1): e48-e70.
- Sayre MR, Koster RW, Botha M, et al. Part 5: adult basic life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2010; 122(16_suppl_2): S298-S324.
- International Liaison Committee on Resuscitation. Part 2. Adult basic life support. 2005 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 2005; 67: 187-200.
About this Guideline

|
Search date/s |
ILCOR literature search details and dates are available on the CoSTR page of the ILCOR website (https://costr.ilcor.org) and the relevant CoSTR documents: Alternative Compression Techniques (BLS 374): Systematic Review https://costr.ilcor.org/document/alternative-compression-techniques-bls-374-tfsr Chest Compression Rate (BLS): Scoping Review https://costr.ilcor.org/document/chest-compression-rate-scoping-review Feedback for CPR Quality (BLS 361): Systematic Review https://costr.ilcor.org/document/feedback-for-cpr-quality-bls-361-tf-sr Firm Surface for CPR (BLS): Systematic Review https://costr.ilcor.org/document/firm-surface-for-cpr-tfsr-costr Hand Position During Compressions (BLS 357): Systematic Review https://costr.ilcor.org/document/hand-position-during-compressions-bls-357-tf-systematic-review Harm for CPR to Victims not in Cardiac arrest (BLS 353): Systematic Review https://costr.ilcor.org/document/harm-from-cpr-to-victims-not-in-cardiac-arrest-tfsr-costr-1 Rescuer Fatigue in CC Only CPR (BLS 349): Scoping Review https://costr.ilcor.org/document/rescuer-fatigue-in-cc-only-cpr-bls-349-scoping-review Starting CPR (ABC vs CAB) (BLS): Systematic Review https://costr.ilcor.org/document/rhythm-check-timing-tfsr-costr |
|
Questions/PICOs: |
Are described in the CoSTR documents (https://costr.ilcor.org) |
|
Method: |
Mixed methods including ARC NHMRC methodology before 2017 and ILCOR GRADE methodology described in ILCOR publications since 2017. |
|
Principal reviewers: |
Julie Considine, Hugh Grantham |
|
Approved: |
April 2021 |
|
Guideline superseded: |
January 2016 |


