Search
Guideline 11.2 – Protocols for Adult Advanced Life Support
Summary
Who does this guideline apply to?
This guideline applies to adults who require advanced life support (ALS).
Who is the audience for this guideline?
This guideline is for health professionals and those who provide healthcare in environments where equipment and drugs are available.
Summary of Recommendations
The 2018 Australian and New Zealand Committee on Resuscitation (ANZCOR) guideline has been reviewed and updated based on evidence reviews including the 20181, 20192 and 20203 International Liaison Committee on Resuscitation (ILCOR) ALS Taskforce evidence reviews. ANZCOR was involved in the ILCOR review and recommendation processes. ANZCOR makes the following recommendations:
- That the Adult ALS algorithm be used as a tool to manage all adults who require advanced life support.
- Good quality cardiopulmonary resuscitation (CPR) and reducing time to defibrillation are the highest priorities in resuscitation from sudden cardiac arrest.
- Rescuers should aim to minimise interruptions to CPR during any ALS intervention.
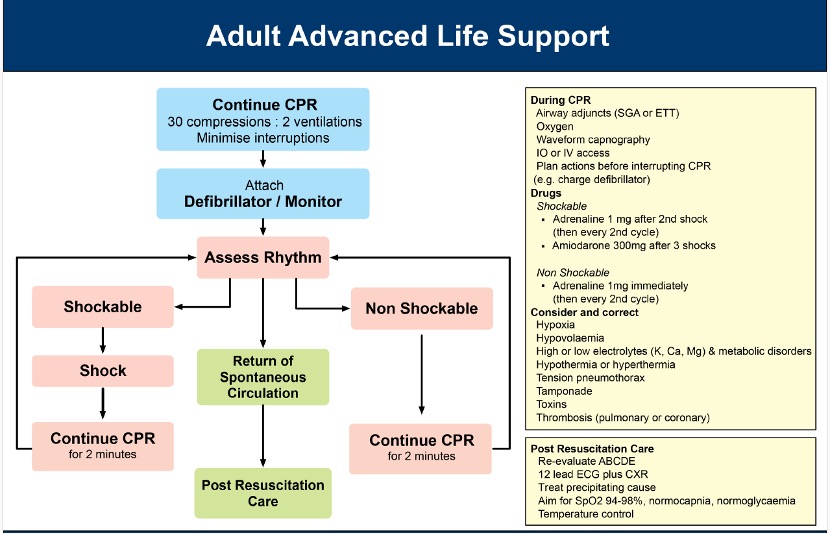
Advanced Life Support Algorithm
The flow diagram illustrates the sequence of actions to be undertaken once equipment and drugs are available. Several tasks in the diagram may be undertaken at the same time.
The algorithm is based on the following considerations:
- The importance of good CPR and early defibrillation in achieving successful outcomes. Ventricular Fibrillation (VF) is, in many situations, the primary rhythm in sudden cardiac arrest. The vast majority of survivors come from this group.
The chance of successful defibrillation decreases with time. Therefore, the performance of good CPR and decreasing the time to defibrillation are the highest priorities in resuscitation from sudden cardiac arrest.
The amplitude and waveform of VF deteriorate as high-energy phosphate stores in the myocardium decrease. This rate of decrease can be slowed, or even reversed by effective basic life support (BLS).4
2. Automated External Defibrillators (AEDs) can accurately diagnose cardiac rhythms and separate them into two groups:
a) Shockable - those responsive to defibrillation.
b)Non-shockable - those unresponsive to defibrillation.
3. There are interventions that are indicated in all causes of cardiac arrest.
4. There is a group of potentially reversible conditions that, if unrecognised or left untreated during cardiac arrest, may prevent successful resuscitation.
Good quality CPR
The provision of good quality CPR is the cornerstone of ALS. This includes delivery of chest compressions over the lower half of the sternum at a depth of at least 5 cm, and at a rate of approximately 100 to 120 per minute, while minimising interruptions to compressions at all times.
Assess rhythm
If using an AED, follow the instructions. If using a manual defibrillator, the pads should be placed on the patient’s chest and, whilst CPR is continued, it should be charged. CPR should then be paused whilst the rhythm is analysed. If a rhythm compatible with spontaneous circulation is observed, the defibrillator should be disarmed and the pulse checked [Good Practice Statement].
Shockable Rhythm
- VF is asynchronous chaotic ventricular activity that produces no cardiac output.
- Pulseless ventricular tachycardia (pVT) is a wide complex regular tachycardia associated with no clinically detectable cardiac output.
- A defibrillator shock should be administered according to the algorithm.
- ANZCOR suggests immediate resumption of chest compressions after shock delivery for adults in cardiac arrest in any setting [CoSTR 2020, weak recommendation, very low certainty evidence]. If there is alternative physiologic evidence of return of spontaneous circulation (ROSC) (e.g., arterial waveform or rapid rise in end tidal carbon dioxide (ETCO2)), chest compressions can be paused briefly for rhythm analysis.5
- ANZCOR suggests against pausing chest compressions at any time interval other than every two minutes to assess the cardiac rhythm [CoSTR 2020, weak recommendation, low quality evidence].5
Energy levels
- Monophasic: the energy level for adults should be set at maximum (usually 360 Joules (J)) for all shocks [Good Practice Statement].6
- Biphasic waveforms: the default initial energy level for adults should be set at 200J. Other energy levels may be used providing there is relevant clinical data for a specific defibrillator that suggests that an alternative energy level provides adequate shock success (e.g., usually greater than 90%) [Good Practice Statement].6
ANZCOR suggests that if the first shock is not successful and the defibrillator is capable of delivering shocks of higher energy, it is reasonable to increase the energy to the maximum available for subsequent shocks [CoSTR 2015 weak recommendation, very low quality evidence].7
Immediate CPR
Interruptions to CPR decrease the chance of survival from cardiac arrest. Whilst defibrillation is of paramount importance for VF/pVT, a period of well performed CPR immediately after each shock can help maintain myocardial and cerebral viability and improve the likelihood of subsequent shock success.4
- During CPR advanced life support interventions are applied and potential causes of arrest sought.
- After each defibrillation, continue a further 2 minutes of CPR unless responsiveness or normal breathing become apparent.
- If using a defibrillator in manual mode, the defibrillator should be charged during CPR, as the end of the 2-minute loop of CPR approaches to minimise interruptions to CPR and increase the likelihood of shock success.3,8
- Rhythm is then reassessed and treatment is directed as necessary. If rhythm assessment results in a significant interruption to CPR, then a further 2 minute period of CPR is recommended before further shocks are delivered. This is done to obtain the benefits of CPR on VF waveform and increase the likelihood of shock success.
- For non-shockable rhythms (pulseless electrical activity (PEA)/asystole), ANZCOR recommends administration of adrenaline (epinephrine) as soon as feasible during CPR (and then every second loop of the ALS algorithm) [CoSTR 2019, strong recommendation, very low certainty of evidence].2
- For shockable rhythms (VF/pVT), ANZCOR suggests administration of adrenaline (epinephrine) after initial defibrillation attempts are unsuccessful during CPR (after 2nd shock and after every second loop of the ALS algorithm) [CoSTR 2019, weak recommendation, very low certainty of evidence].2
- ANZCOR suggests the use of amiodarone in adults with shock-refractory VF/pVT (directly after the 3rd shock) [CoSTR 2018, weak recommendation, low quality evidence].1
- Therefore, sequence of escalating advanced life support is:
- Attempt defibrillation, and ensure good CPR.
- Attempt defibrillation, and add vasopressor (adrenaline 1mg).
- Attempt defibrillation, and add anti-arrhythmic (amiodarone 300mg).
Non-shockable rhythm (Non VF/VT)
- Asystole is characterised by the absence of any cardiac electrical activity.
- Pulseless Electrical Activity (PEA) (sometimes referred to as Electromechanical Dissociation (EMD)) is the presence of a coordinated electrical rhythm without a detectable cardiac output.
- The prognosis with PEA or asystole is much less favourable than with VF/pVT.
- During CPR, ALS interventions are applied and potential causes of arrest sought.
- Defibrillation is not indicated and the emphasis is on CPR and other ALS interventions (e.g., intravenous access, consideration of advanced airway, drugs, pacing and correcting reversible causes) [Good Practice Statement].
During CPR
The following interventions apply to all rhythms and are carried out continuously or during each loop of the algorithm. Each loop comprises 5 sets of 30 compressions (at approximately 100 to120 per minute) to 2 breaths (30:2), which equates to approximately 2 minutes. Rhythms changing from shockable to non-shockable (and vice versa) during the same resuscitation result in switching to the appropriate limb of the algorithm.
Other management priorities during CPR:
- Minimise interruptions to CPR during ALS interventions.
- ANZCOR suggests administering 100% oxygen when available [CoSTR 2015 weak recommendation, very low quality evidence].7
- ANZCOR suggests intravenous (IV) access is the preferred means of administering medications to patients during or after cardiac arrest, when compared to intraosseous (IO) access [CoSTR 2020, weak recommendation, very low certainty evidence].3
- ANZCOR suggests if attempts at IV access are unsuccessful or not feasible, IO access should be used [CoSTR 2020, weak recommendation, very low certainty evidence].3
- Consider airway adjuncts (e.g., supraglottic airway (SGA) or endotracheal tube (ETT)), but attempts to secure the airway should not interrupt CPR for more than 5 seconds [Good Practice Statement].
- ANZCOR recommends waveform capnography should be used to confirm airway placement and monitor the adequacy of CPR [CoSTR 2015 strong recommendation, low quality evidence].7
- ANZCOR recommends that adrenaline (epinephrine) should be administered every second loop (approximately every 4 minutes) [CoSTR 2019, strong recommendation, very low certainty of evidence].2
- Other drugs/electrolytes should be considered depending on the individual circumstances [Good Practice Statement].
Medications during CPR
2.8.1 Vasopressors
Giving vasopressor drugs routinely during human cardiac arrest has not been shown to increase the rate of neurologically intact survival to hospital discharge. It is however reasonable to continue to use vasopressor drugs on a routine basis to achieve ROSC and provide the opportunity for additional therapies to potentially improve outcomes.
For non-shockable rhythms (PEA/asystole), ANZCOR recommends administration of adrenaline (epinephrine) as soon as feasible during CPR (and then every second loop of the ALS algorithm) [CoSTR 2019, strong recommendation, very low certainty of evidence].2
For shockable rhythms (VF/pVT), ANZCOR suggests administration of adrenaline (epinephrine) if 2 initial defibrillation attempts are unsuccessful during CPR (after 2nd shock and after every second loop of the ALS algorithm) [CoSTR 2019, weak recommendation, very low certainty of evidence].2
2.8.2 Antiarrhythmic drugs
Giving antiarrhythmic drugs routinely during cardiac arrest has not been shown to increase the rate of neurologically intact survival to hospital discharge. It is however reasonable to continue to use antiarrhythmic drugs on a routine basis to achieve ROSC and provide the opportunity for additional therapies to potentially improve outcomes.
ANZCOR suggests the use of amiodarone in adults with shock-refractory VF/pVT (directly after the 3rd shock) [CoSTR 2018, weak recommendation, low-quality evidence].1
ANZCOR suggests lidocaine (lignocaine) may be used as an alternative to amiodarone in adults with shock-refractory VF/pVT [CoSTR 2018, weak recommendation, low-quality evidence].1
2.8.3 Other drugs
There is no evidence that routinely administering other drugs (e.g., buffers, atropine, calcium, magnesium) during human cardiac arrest increases survival to hospital discharge.9 There may be specific circumstances where other drugs are indicated (e.g., toxins, hyperkalaemia, known QT abnormalities, pulmonary embolism) (Refer to ANZCOR Guideline 11.5 Medications in Adult Cardiac Arrest).
Correct Reversible Causes
Very few data addresses the aetiology of cardiac arrest directly. One prospective study and one retrospective study suggested that rescuers can identify some non-cardiac causes of some arrests.10,11 The physical circumstances, history, precipitating events, clinical examination, or the use of adjunct techniques (such as ultrasound) may enable the rescuer to determine a cardiac or non-cardiac cause of the cardiorespiratory arrest. The rescuer should undertake interventions based on the presumed aetiology (cardiac or non-cardiac).
4 Hs and 4 Ts are a simple reminder of conditions that may precipitate cardiac arrest or decrease the chances of successful resuscitation. These conditions should be sought and, if present, corrected in every case.
- Hypoxaemia
- Hypovolaemia
- Hyper/hypokalaemia & metabolic disorders
- Hypo/hyperthermia
- Tension pneumothorax
- Tamponade
- Toxins / poisons / drugs
- Thrombosis-pulmonary / coronary
2.9.1 Fluid administration
Fluids should be infused if hypovolemia is suspected (hypovolaemic shock would normally require the administration of at least 20 mL/kg crystalloid solution (e.g., 0.9% sodium chloride solution) [Good Practice Statement].
2.9.2 Thrombolytics
Routine administration of fibrinolytics for the treatment of in-hospital and out-of hospital cardiac arrest is not recommended [Good Practice Statement].
ANZCOR suggests administering fibrinolytic drugs for cardiac arrest when pulmonary embolism (PE) is the suspected cause of cardiac arrest [CoSTR 2020, weak recommendation, very low-certainty evidence].3
ANZCOR suggests the use of fibrinolytic drugs or surgical embolectomy or percutaneous mechanical thrombectomy for cardiac arrest when PE is the known cause of cardiac arrest [CoSTR 2020, weak recommendation, very low-certainty evidence].3
Checking Resuscitation Equipment
ANZCOR guidelines should be considered in conjunction with accepted National Standards and local policies. ANZCOR is aware of cases where equipment failure (e.g. oxygen pipes being incorrectly connected resulting in hypoxic gases being administered, and resuscitation bag valve devices incorrectly assembled) has led to adverse outcomes.
The checking and maintenance of hospital and resuscitation equipment is covered by National Standards and local policies. Practitioners involved in resuscitation should always be alert to errors of assembly or use, and have checking processes to minimise these risks before equipment is used. They should also respond to unexpected situations with further checking procedures, and in the case of unexplained hypoxia change gas supply and circuits, and may include removing the patient from ventilators and gas supplies by using a self-inflating bag with room air. In this situation oxygen analysis of delivered gases should be considered and an oxygen analyser should be available [Good Practice Statement].
Post Resuscitation Care
After ROSC, post-resuscitation care commences (Refer to ANZCOR Guideline 11.7 and 11.8).
Re-evaluate the patient using the standard ABCDE approach: Airway, Breathing, Circulation, Disability and Exposure.
Other considerations include obtaining a 12 lead ECG and a chest radiograph. The adequacy of perfusion should be assessed, and the need for reperfusion therapy should be considered (e.g., thrombolytics or percutaneous coronary intervention). The adequacy of oxygenation and ventilation should be confirmed and maintained (an advanced airway may be required).
Post resuscitation temperature control should be instituted if indicated. Further investigation for reversible causes should be continued, and treatment instituted where necessary (Refer to ANZCOR Guideline 11.7 and 11.8).
Abbreviations
|
Abbreviation |
Meaning/Phrase |
|
AED |
automated external defibrillator |
|
ALS |
advanced life support |
|
ANZCOR |
Australian and New Zealand Committee on Resuscitation |
|
ARC |
Australian Resuscitation Council |
|
BLS |
basic life support |
|
CoSTR |
Consensus on Science with Treatment Recommendations |
|
CPR |
cardiopulmonary resuscitation |
|
EMD |
electromechanical dissociation |
|
ETCO2 |
end tidal carbondioxide |
|
ETT |
endotracheal tube |
|
ILCOR |
International Liaison Committee on Resuscitation |
|
IO |
intraosseus |
|
IV |
intravenous |
|
J |
joules |
|
PE |
pulmonary embolism |
|
PEA |
pulseless electrical activity |
|
pVT |
pulseless ventricular tachycardia |
|
ROSC |
return of spontaneous circulation |
|
SGA |
supraglottic airway |
|
VF |
ventricular fibrillation |
References
- Soar J, Donnino MW, Maconochie I, Aickin R, Atkins DL, Andersen LW, Berg KM, Bingham R, Bottiger BW, Callaway CW, et al; on behalf of the ILCOR Collaborators. 2018 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations summary. Resuscitation. 2018;133:194–206. doi:23 10.1016/j.resuscitation.2018.10.017
- Soar J, Maconochie I, Wyckoff MH, et al. 2019 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces.Resuscitation 2019; https://doi.org/10.1016/j.resuscitation.2019.10.016
- Soar J, Berg KM, Andersen LW et al. 4: Adult Advanced Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2020;156:A80-A119. https://doi.org/10.1016/j.resuscitation.2020.09.012
- Eftestol T, Wik L, Sunde K, Steen PA. Effects of Cardiopulmonary Resuscitation on Predictors of Ventricular Fibrillation Defibrillation Success During Out-of-Hospital Cardiac Arrest. Circulation. 2004 June 21;110:10-5.
- Olasveengen TM, Mancini ME, Perkins GD et al on behalf of the Adult Basic Life Support Collaborators. Adult Basic Life Support. 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2020;156:A35-79.
- Sunde K, Jacobs I, Deakin CD, Hazinski MF, Kerber RE, Koster RW, et al. Part 6: Defibrillation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. [doi: DOI: 10.1016/j.resuscitation.2010.08.025]. 2010;81(1, Supplement 1):e71-e85.
- Soar J, Callaway C, Aibiki M, Böttiger BW, Brooks SC, Deakin CD, Donnino MW, Drajer S, Kloeck W, Morley PT, Morrison LJ, Neumar RW, Nicholson TC, Nolan JP, Okada K, O’Neil BJ, Paiva EF, Parr MJ, Wang TL, Witt J, on behalf of the Advanced Life Support Chapter Collaborators. Part 4: Advanced life support. 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2015;95:e71–e120
- Edelson DP, Robertson-Dick BJ, Yuen TC, Eilevstjonn J, Walsh D, Bareis CJ, et al. Safety and efficacy of defibrillator charging during ongoing chest compressions: a multi-center study. Resuscitation. 2010 Nov;81(11):1521-6.
- Deakin CD, Morrison LJ, Morley PT, Callaway CW, Kerber RE, Kronick SL, et al. Part 8: Advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2010;81(1, Supplement 1):e93-e174. [doi:10.1016/j.resuscitation.2010.08.027]
- Pell JP, Sirel JM, Marsden AK, Ford I, Walker NL, Cobbe SM. Presentation, management, and outcome of out of hospital cardiopulmonary arrest: comparison by underlying aetiology. Heart (British Cardiac Society) 2003;89(8):839-42
- Kuisma M, Alaspaa A. Out-of-hospital cardiac arrests of non-cardiac origin: epidemiology and outcome. Eur Heart J 1997;18(7):1122-1128.
ANZCOR ALS Algorithm
About this Guideline
Search date/s |
ILCOR literature search details and dates are available on the CoSTR page of the ILCOR website (https://costr.ilcor.org) and the relevant CoSTR documents: https://costr.ilcor.org/document/antiarrhythmic-drugs-for-cardiac-arrest-adults https://costr.ilcor.org/document/vasopressors-in-adult-cardiac-arrest |
|
Questions/PICOs: |
Are described in the CoSTR documents (https://costr.ilcor.org) |
|
Method: |
Mixed methods including ARC NHMRC methodology before 2017 and ILCOR GRADE methodology described in ILCOR publications since 2017. |
|
Principal reviewers: |
Michael Parr; Margaret Nicholson, Tonia Nicholson |
|
Major changes from previous Guideline |
No major changes. Updated using terminology consistent with current ILCOR evidence review processes. |
|
Other Consultation: |
|
|
Approved: |
June 2024 |
|
Guidelines Superseded: |
August 2018 |
Referencing this guideline
When citing the ANZCOR Guidelines we recommend:
ANZCOR, 2026, Guideline 11.2 – Protocols for Adult Advanced Life Support, accessed 5 March 2026, https://www.anzcor.org/home/adult-advanced-life-support/guideline-11-2-protocols-for-adult-advanced-life-support



