Search
Guideline 13.6 – Chest Compressions during Resuscitation of the Newborn
Next review July 2024
Summary

ANZCOR Guidelines 13.1 to 13.10 and the Newborn Life Support algorithm are provided to assist in the resuscitation of newborn infants. Differences from the adult and paediatric guidelines reflect differences in the anatomy and physiology and the causes of cardiorespiratory arrest for newborns, older infants, children and adults. These guidelines draw from Neonatal Life Support 2020 and 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations (CoSTR) 1, 2 the development of which included representation from ANZCOR. The 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Care 3 and local practices have also been taken into account.
To whom do these guidelines apply?
The term ‘newborn’ or ‘newborn infant’ refers to the infant in the first minutes to hours following birth. In contrast, the neonatal period is defined as the first 28 days of life. Infancy includes the neonatal period and extends through the first 12 months of life.
ANZCOR Guidelines 13.1 to 13.10 and the Newborn Life Support algorithm are mainly for the care of newborns. The exact age at which paediatric techniques and in particular, compression-ventilation ratios, should replace the techniques recommended for newborns is unknown, especially in the case of very small preterm infants. For term infants beyond the first minutes to hours following birth, and particularly in those with known or suspected cardiac aetiology of their arrest, paediatric techniques may be used. (Refer to Paediatric Advanced Life Support ANZCOR Guidelines 12.1 to 12.7).
Who is the audience for these guidelines?
ANZCOR Guidelines 13.1 to 13.10 and the Newborn Life Support algorithm are for health professionals and those who provide healthcare in environments where equipment and drugs are available (such as a hospital). When parents are taught CPR for their infants who are being discharged from birth hospitals, the information in Basic Life Support Guidelines (ANZCOR Guidelines 2 to 8) is appropriate.
Recommendations
The Australian and New Zealand Committee on Resuscitation (ANZCOR) makes the following recommendations:
- Because ventilation is the most effective action in newborn resuscitation and because chest compressions are likely to compete with the performance and assessment of effective ventilation, resuscitators should ensure that assisted ventilation is being delivered optimally before starting chest compressions. [Good Practice Statement]
- Once compressions are started, they should be continued with as little interruption as possible until there is clear evidence of improvement in spontaneous heart rate. [Good Practice Statement]
- As soon as a decision has been made to perform chest compressions, preparation should commence to establish vascular access and administer intravenous adrenaline (epinephrine). [Good Practice Statement]
- Chest compressions should be centred over the lower third of the sternum (above the xiphisternum and just below the nipples) and should compress the chest one third of the chest anterior-posterior diameter. [Good practice statement, extrapolated evidence]
- ANZCOR suggests a technique using two thumbs on the lower third of the sternum, superimposed or adjacent to each other according to the size of the infant, with the fingers surrounding the thorax to support the back. [CoSTR 2015 and 2020, Weak recommendation, very low certainty of evidence]
- ANZCOR suggests the two-thumb technique over the two-finger technique because it achieves superior peak systolic and coronary perfusion pressure, provides compressions more consistently over long periods of time, and it is easier and less tiring for the resuscitator. [CoSTR 2015, Weak recommendation, very low certainty of evidence] The only circumstance in which the two-finger technique should be considered is when only a single resuscitator is available. [Good Practice Statement]
- ANZCOR suggests that inflations and chest compressions should be performed with a 3:1 ratio of 90 compressions per minute and a half second pause after each 3rd compression to deliver an inflation. [CoSTR 2015, weak recommendation, very low certainty of evidence] Compressions and inflations should be coordinated to avoid simultaneous delivery of a compression and a breath. (Good practice statement, extrapolated evidence] Continuous chest compressions at 120 compressions per minute without interruptions for breaths can be considered in the intubated newborn. [Good Practice Statement]
- The chest should fully expand between compressions, but the rescuer’s hands should not leave the chest. [Good Practice Statement]
- As soon as chest compressions are commenced, it is usual practice to increase inspired oxygen to 100% if a lower concentration has previously been used. ANZCOR suggests that if 100% oxygen is used then it should be weaned as soon as possible after the heart rate has recovered. [CoSTR 2015 and 2020, Weak recommendation, very low certainty of evidence]
- Once chest compressions have been commenced, they should be performed with as little interruption as possible. Do not stop unless assessment is needed to make treatment decisions. Signs of improvement in spontaneous cardiac output may include improvement in spontaneous heart rate, a rise in oxygen saturation, and commencement of some spontaneous movement or breaths. Chest compressions should continue until it is obvious that the heart rate is >60 beats per minute. [Good Practice Statements]
Abbreviations
|
Abbreviation |
Meaning/Phrase |
|
ANZCOR |
Australian and New Zealand Committee on Resuscitation |
|
CI |
Confidence interval (95%) |
|
CoSTR |
International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations |
|
CPR |
Cardiopulmonary resuscitation |
Guideline

The normal newborn has a heart rate above 100 beats per min once breathing has been established, usually within two minutes of birth..4 The normal range of heart rate thereafter is 110 to 160 beats per minute..4 In newborns cardiac output is rate dependent. If the heart rate is too slow the circulation will be inadequate to support tissue oxygenation.
Indications for starting chest compressions

Chest compressions are indicated when the heart rate is <60 beats per minute despite adequate assisted ventilation provided for 30 seconds (chest wall obviously moving with each inflation).
Because ventilation is the most effective action in newborn resuscitation and because chest compressions are likely to compete with the performance and assessment of effective ventilation, resuscitators should ensure that assisted ventilation is being delivered optimally before starting chest compressions. 1 [Good Practice Statement]
Once compressions are started, they should be continued with as little interruption as possible until there is clear evidence of improvement in spontaneous heart rate. [Good Practice Statement]
As soon as a decision has been made to perform chest compressions, preparation should commence to establish vascular access and administer intravenous adrenaline (epinephrine). [Good Practice Statement] Refer to ANZCOR Guideline 13.7.
Chest compression technique

Chest compressions should be centred over the lower third of the sternum (above the xiphisternum and just below the nipples)2, 5 and should compress the chest one third of the chest anterior-posterior diameter. 5, 6 [Good practice statement, extrapolated evidence]
ANZCOR suggests a technique using two thumbs on the lower third of the sternum, superimposed or adjacent to each other according to the size of the infant, with the fingers surrounding the thorax to support the back. 1, 2 [CoSTR 2015 and 2020, Weak recommendation, very low certainty of evidence]
Usually, the resuscitator faces the newborn’s head (figure 1), but in special circumstances, such as when access is needed to the newborn’s abdomen, this position can be reversed (figure 2). 2
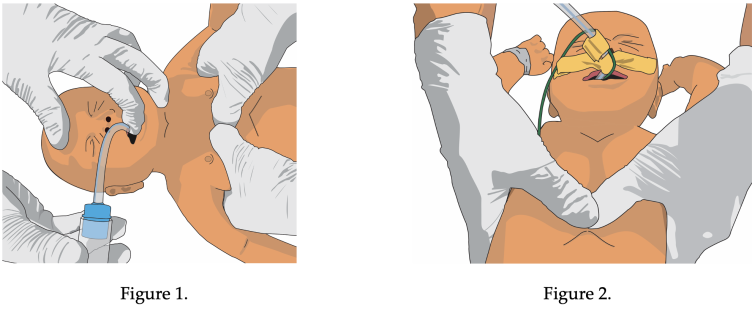
ANZCOR suggests the two-thumb technique over the two-finger technique because it achieves superior peak systolic and coronary perfusion pressure, provides compressions more consistently over long periods of time, and it is easier and less tiring for the resuscitator. 2 [CoSTR 2015, Weak recommendation, very low certainty of evidence] The only circumstance in which the two-finger technique should be considered is when only a single resuscitator is available. [Good Practice Statement]
ANZCOR suggests that inflations and chest compressions should be performed with a 3:1 ratio of 90 compressions per minute and a half second pause after each 3rd compression to deliver an inflation. 2 [CoSTR 2015, Weak recommendation, very low certainty of evidence] Compressions and inflations should be coordinated to avoid simultaneous delivery of a compression and a breath. 2 [extrapolated evidence] There is no compelling evidence suggesting a benefit to other ratios for the newborn. Since asphyxia is the predominant cause of cardiovascular collapse in the newborn, effective resuscitation requires significant focus on ventilation. 2 Continuous chest compressions at 120 compressions per minute without interruptions for breaths can be considered in the intubated newborn. [Good Practice Statement]
The chest should fully expand between compressions, 7 but the rescuer’s hands should not leave the chest. 2 [Good Practice Statement]
Oxygen During Chest Compressions

Effectively delivered chest compressions will result in pulsations evident on an oximeter. As soon as chest compressions are commenced, it is usual practice to increase inspired oxygen to 100% if a lower concentration has previously been used. By the time chest compressions are deemed to be needed, then the steps of trying to achieve return of spontaneous circulation with lower oxygen concentrations should already have been attempted and would have failed to increase the heart rate. Thus, it seems prudent to try increasing the supplementary oxygen concentration. However, animal studies show no advantage of 100% oxygen over air in terms of return of spontaneous circulation in these circumstances and there are no human studies. ANZCOR suggests that if 100% oxygen is used then it should be weaned as soon as possible after the heart rate has recovered. 1, 2 [CoSTR 2015 and 2020, weak recommendation, very low certainty of evidence]
References

- Wyckoff MH, Wyllie J, Aziz K, de Almeida MF, Fabres JW, Fawke J, et al. Neonatal Life Support 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation. 2020;156:A156-A87.
- Wyllie J, Perlman JM, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R, et al. Part 7: Neonatal resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2015;95:e169-201.
- Aziz K, Lee HC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS, et al. Part 5: Neonatal Resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S524-s50.
- Dawson J, Kamlin C, Wong C, te Pas A, Vento M, Cole T, et al. Changes in heart rate in the first minutes after birth. Archives of Disease in Childhood - Fetal and Neonatal Edition. 2010;95(3):F177-F81.
- Orlowski JP. Optimum position for external cardiac compression in infants and young children. Ann Emerg Med. 1986;15(6):667-73.
- Phillips GW, Zideman DA. Relation of infant heart to sternum: its significance in cardiopulmonary resuscitation. Lancet. 1986;1(8488):1024-5.
- Meyer A, Nadkarni V, Pollock A, Babbs C, Nishisaki A, Braga M, et al. Evaluation of the Neonatal Resuscitation Program's recommended chest compression depth using computerized tomography imaging. Resuscitation. 2010;81(5):544-8.
About this Guideline

Search date/s |
ILCOR literature search details and dates are available on the CoSTR page of the ILCOR website (https://costr.ilcor.org) and the relevant CoSTR documents. 1, 2 |
|
Questions/PICOs: |
Are described in the CoSTR documents (https://costr.ilcor.org) |
|
Method: |
Mixed methods including ARC NHMRC methodology before 2017 and ILCOR GRADE methodology described in ILCOR publications since 2017. |
|
Principal reviewers: |
Helen Liley, Lindsay Mildenhall, Marta Thio, Callum Gately |
|
Main changes |
Updating of review evidence, references, and terminology to increase consistency with GRADE terminology. |
|
Approved: |
April 2021 |


